Doccol MCAO Sutures Reduce SD to 5% of Its Corresponding Mean Value for Infarction Volume
In the stroke model literature, two types of MCAO (middle cerebral artery occlusion) models are most frequently used, which are the Koizumi model (Koizumi et al. 1986), and the Longa model (Longa et al. 1989). The Koizumi model suggested the use of silicone rubber-coated monofilaments as occludors whilst the Longa model used flame-blunted monofilaments. It turned out that silicone rubber-coated monofilaments are superior to flame-blunted monofilaments for producing consistent ischemic brain injuries. A study (Tsuchiya et al. 2003) showed that using flame-blunted monofilaments for inducing MCA occlusion caused 40% occurrence of subarachnoid hemorrhage, and the standard deviation for infarction volume was greater than its corresponding mean value. Another technical paper specifically compared the effects of suture types on the infarct consistency and showed that silicone rubber-coated monofilaments were superior to flame-blunted ones, producing consistent infarction; and this was true even with inexperienced surgeons. (Shimamura et al. 2006a) In the mouse intraluminal model, SAH rate could reach 40% if uncoated heat-blunted monofilaments being used; and such a modeling method resulted in the deviation for infarction volume being larger than 50% of its corresponding mean value. (Tsuchiya et al. 2003) The poly-L-Lysine coated monofilament seemed could only increase the mortality (to a rate of 60%), without any benefits for reducing infarct variation. (Huang et al. 1998)
The mechanism behind the outcome variation is the frequent occurrence of insufficient occlusion, premature reperfusion, and filament dislodgement. Doccol MCAO sutures have a sufficient length of coated surface, which is cylindrical in shape, elastic, and smooth. Doccol MCAO sutures, with such a physical property and huge selections for different coating diameters and coating length, are able to reduce the occurrence of the insufficient occlusion, the premature reperfusion, and the monofilament dislodgement.
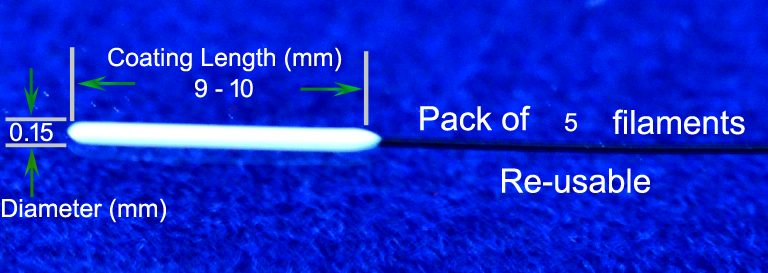
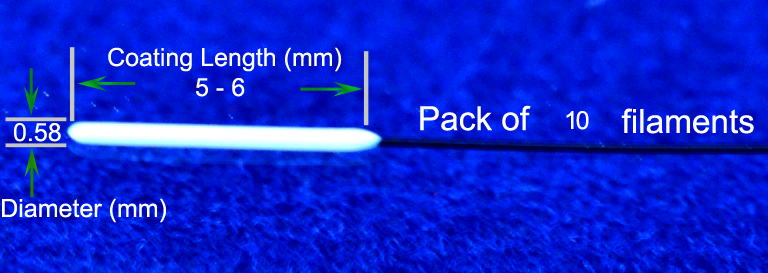
The standard deviation for infarction volume, when home-made silicone rubber-coated monofilaments being used, is around 30% of its corresponding mean value both in rats (Schmid-Elsaesser et al. 1998) and in mice (Shah et al. 2006). The use of Doccol MCAO sutures has been reported to be able to achieve a much better result. For examples, a 15-min occlusion by using home-prepared monofilaments usually produces no apparent ischemic damage whilst a consistent caudate infarction can be achieved when Doccol MCAO sutures being used; (Pignataro et al. 2007a) The standard deviation for infarction volume is around 10% to 20% of its corresponding mean values for 60-min transient to 24-h permanent occlusions in rats, (Candelario-Jalil et al. 2008; Khan et al. 2006; Liu et al. 2006; Shimamura et al. 2006b; Solaroglu et al. 2006; Tsubokawa et al. 2007; Tsubokawa et al. 2006a; Tsubokawa et al. 2006b) and around 5-10% of its corresponding mean value for the 60-min occlusion in mice, (Kleinschnitz et al. 2007; Maysami et al. 2008; Pignataro et al. 2007b; Pignataro et al. 2007c) when Doccol MCAO sutures being used. Some variation in infarct volumes may be contributed by the differences of experimental design and the selection of the right-sized monofilaments.
References
1. Candelario-Jalil E, Munoz E, Fiebich BL. (2008) Detrimental effects of tropisetron on permanent ischemic stroke in the rat. BMC Neurosci 9:19
2. Huang J, Kim LJ, Poisik A, Pinsky DJ, Connolly ES, Jr. (1998) Does poly-L-lysine coating of the middle cerebral artery occlusion suture improve infarct consistency in a murine model? J Stroke Cerebrovasc Dis 7:296-301
3. Khan M, Jatana M, Elango C, Paintlia AS, Singh AK, Singh I. (2006) Cerebrovascular protection by various nitric oxide donors in rats after experimental stroke. Nitric Oxide 15:114-124
4. Kleinschnitz C, Pozgajova M, Pham M, Bendszus M, Nieswandt B, Stoll G. (2007) Targeting platelets in acute experimental stroke: impact of glycoprotein Ib, VI, and IIb/IIIa blockade on infarct size, functional outcome, and intracranial bleeding. Circulation 115:2323-2330
5. Koizumi J, Yoshida Y, Nakazawa T, Ooneda G. (1986) Experimental studies of ischemic brain edema, I: a new experimental model of cerebral embolism in rats in which recirculation can be introduced in the ischemic area. Jpn J Stroke 8:1-8
6. Liu S, Liu W, Ding W, Miyake M, Rosenberg GA, Liu KJ. (2006) Electron paramagnetic resonance-guided normobaric hyperoxia treatment protects the brain by maintaining penumbral oxygenation in a rat model of transient focal cerebral ischemia. J Cereb Blood Flow Metab 26:1274-1284
7. Longa EZ, Weinstein PR, Carlson S, Cummins R. (1989) Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke 20:84-91
8. Maysami S, Lan JQ, Minami M, Simon RP. (2008) Proliferating progenitor cells: a required cellular element for induction of ischemic tolerance in the brain. J Cereb Blood Flow Metab 28:1104-1113
9. Pignataro G, Simon RP, Boison D. (2007a) Transgenic overexpression of adenosine kinase aggravates cell death in ischemia. J Cereb Blood Flow Metab 27:1-5
10. Pignataro G, Simon RP, Xiong ZG. (2007b) Prolonged activation of ASIC1a and the time window for neuroprotection in cerebral ischaemia. Brain 130:151-158
11. Pignataro G, Studer FE, Wilz A, Simon RP, Boison D. (2007c) Neuroprotection in ischemic mouse brain induced by stem cell-derived brain implants. J Cereb Blood Flow Metab 27:919-927
12. Schmid-Elsaesser R, Zausinger S, Hungerhuber E, Baethmann A, Reulen HJ. (1998) A critical reevaluation of the intraluminal thread model of focal cerebral ischemia: evidence of inadvertent premature reperfusion and subarachnoid hemorrhage in rats by laser-Doppler flowmetry. Stroke 29:2162-2170
13. Shah ZA, Namiranian K, Klaus J, Kibler K, Dore S. (2006) Use of an optimized transient occlusion of the middle cerebral artery protocol for the mouse stroke model. J Stroke Cerebrovasc Dis 15:133-138
14. Shimamura N, Matchett G, Tsubokawa T, Ohkuma H, Zhang J. (2006a) Comparison of silicone-coated nylon suture to plain nylon suture in the rat middle cerebral artery occlusion model. J Neurosci Methods 156:161-165
15. Shimamura N, Matchett G, Yatsushige H, Calvert JW, Ohkuma H, Zhang J. (2006b) Inhibition of integrin alphavbeta3 ameliorates focal cerebral ischemic damage in the rat middle cerebral artery occlusion model. Stroke 37:1902-1909
16. Solaroglu I, Tsubokawa T, Cahill J, Zhang JH. (2006) Anti-apoptotic effect of granulocyte-colony stimulating factor after focal cerebral ischemia in the rat. Neuroscience 143:965-974
17. Tsubokawa T, Jadhav V, Solaroglu I, Shiokawa Y, Konishi Y, Zhang JH. (2007) Lecithinized superoxide dismutase improves outcomes and attenuates focal cerebral ischemic injury via antiapoptotic mechanisms in rats. Stroke 38:1057-1062
18. Tsubokawa T, Solaroglu I, Yatsushige H, Cahill J, Yata K, Zhang JH. (2006a) Cathepsin and calpain inhibitor E64d attenuates matrix metalloproteinase-9 activity after focal cerebral ischemia in rats. Stroke 37:1888-1894
19. Tsubokawa T, Yamaguchi-Okada M, Calvert JW, Solaroglu I, Shimamura N, Yata K, Zhang JH. (2006b) Neurovascular and neuronal protection by E64d after focal cerebral ischemia in rats. J Neurosci Res 84:832-840
20. Tsuchiya D, Hong S, Kayama T, Panter SS, Weinstein PR. (2003) Effect of suture size and carotid clip application upon blood flow and infarct volume after permanent and temporary middle cerebral artery occlusion in mice. Brain Res 970:131-139 |

